
Get the booklet
Download Feeling Low or Anxious after a brain injury in pdf format
Feeling low or anxious
Low mood and depression
Everyone experiences periods of sadness or feeling low at some point in their life. This is particularly common after an injury or illness such as a brain injury. A brain injury usually happens unexpectedly and may have brought significant changes to your life. The injury is often accompanied by loss – loss of skills, independence and even livelihood.
You may also be experiencing a lot of uncertainty about how full a recovery you will make. It is normal to feel a range of emotions including sadness, in response to these changes and losses.
There are many symptoms of low mood including:
- Feeling tired.
- Feeling sad.
- Feeling bad about yourself (low self-esteem).
Feeling frustrated, irritable or angry. There are a number of reasons why after a brain injury you may feel low; these include the low mood being the direct result of the specific area of the brain that was damaged or if you are coming to realise the full extent to which life has changed. If you are feeling low, tell someone you trust and try the What you can do tips. If you do not start to feel any better, arrange to visit your GP.
There are a number of reasons why after a brain injury you may feel low; these include the low mood being the direct result of the specific area of the brain that was damaged or if you are coming to realise the full extent to which life has changed.
If you are feeling low, tell someone you trust and try the What you can do tips below. If you do not start to feel any better, arrange to visit your GP.
Depression
What is the difference between low mood and depression?
The main differences between low mood and depression are the length of time the symptoms last and the impact the symptoms have on your day-to-day life. Having inescapable feelings of sadness and getting little or no pleasure out of things you used to enjoy are key features of depression. If you have these feelings nearly all of the time for at least two weeks you may be experiencing depression.
Symptoms of depression include:
- Lack of interest in things you used to enjoy.
- Tiredness or reduced energy.
- Feeling sad, hopeless, worthless or guilty.
- Change in libido (sex drive).
- Changes in sleep patterns.
- Withdrawing from other people.
- Poor concentration.
- Irritability.
- Changes in weight or eating patterns.
- Thinking about death or suicide.

Having one, or a number, of the symptoms of depression does not necessarily mean you are depressed. Talk to your GP if you are concerned.
If you have strong thoughts of ending your life or harming yourself: tell someone you trust, phone your GP or text ‘help’ to 51444, phone the Samaritans on t: 116 123 or phone Pieta House on 1800 247 247, call 999 or go to Accident and Emergency.
Why does depression happen after a brain injury?
Why does depression happen after a brain injury?
There are a number of possible reasons including:
- Changes in the brain directly due to the injury. If the areas of the brain involved in managing emotions are damaged, this may lead to depression.
- Emotional reaction to the injury – a brain injury is a traumatic change which can result in disability and changes in roles and relationships. Becoming aware of these changes, and trying to adjust to them, can feel overwhelming and may contribute to depression.
- Psychological changes after the brain injury such as being less able to deal with frustration, having less self-awareness, lowered self-confidence and self-esteem or having unrealistic expectations about recovery, may also contribute to depression.
- Reasons unrelated to the brain injury – you will have had many different life experiences prior to your brain injury. These experiences can influence how you respond to, and cope with, difficult life events.
Stress and anxiety
Stress is the way we feel when we are dealing with demands. These can be everyday demands such as looking after children or commuting. Some stress is good and allows us to perform at our best when we need to – for example when we are doing an interview. Other things that cause stress can be exciting – for example skydiving or riding a roller coaster.
However, the stress from some demands and situations can make us feel as if we cannot cope. A life-changing event such as a brain injury may make us feel overwhelmed. Stress can build up over time and may be accompanied by feelings of anxiety
Anxiety explained
Anxiety is a normal human reaction and everyone experiences it at times. It can trigger an alarm and survival response in our body. This is sometimes called the ‘Fight – Flight – Freeze’ response. This response can be switched on when we feel threatened or in danger. Stress hormones are released into our blood in order to prepare us to fight, flee or freeze (stay still).
The anxiety response causes a number of changes in our body:
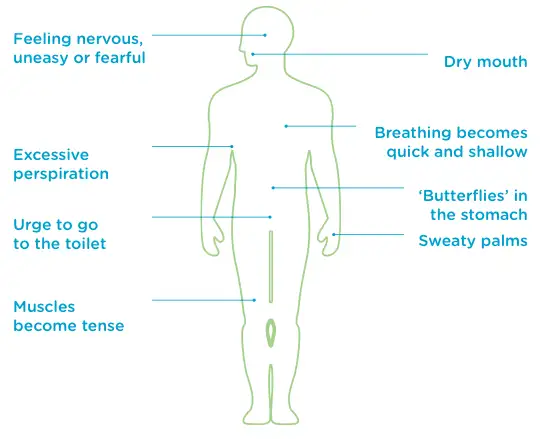
All of these changes happen to help keep us safe from danger. Sometimes our anxiety response is switched on when we think we are in danger but are not actually in danger – for example when speaking in public or meeting a group of people we don’t know. When our anxiety response is activated and there is no real danger, it can be uncomfortable and unpleasant. It can be accompanied by thoughts of being in danger, that something bad is going to happen and a feeling of being unable to cope.
If anxiety is affecting what you do in your day-to-day life, try the What you can do tips below and consider contacting your GP.
What causes anxiety after a brain injury?
Anxiety is a common reaction after a brain injury.
- Lots of things may be more difficult now – for example being in crowded and noisy surroundings may be overwhelming and lead to anxiety.
- If you now have difficulty with reasoning or problem solving, making everyday decisions may be difficult and may make you overly anxious.
- If you try to do too much, too soon or give yourself an unrealistic time frame for recovery, your anxiety levels may go up if you don’t meet these goals.
How common are depression and anxiety after a brain injury?
- A recent piece of research by the Royal College of Surgeons in Ireland (RCSI) showed that 32% of stroke survivors suffered significant anxiety.
- Approximately 30% of people experience depression following a Traumatic Brain Injury (TBI) and roughly half of stroke survivors.
- If you had depression or anxiety before your brain injury, you have a higher risk of experiencing them after the injury.
What you can do
We have listed below things to try yourself that may help alleviate symptoms of depression, feeling low or anxiety.
- Get into a routine and keep active – a brain injury may bring major disruption to daily routines such as work or social activities. Getting back into some form of a routine, spending time with friends, family and acquaintances, as well as doing activities, can help in managing low mood. Try activities and hobbies you once enjoyed. If these are no longer possible, try to find new ones you might enjoy.
- Talk to someone – sharing your thoughts with someone else can help you to gain perspective and help to make life feel more manageable. You could also try writing down how you feel. This may help you identify what is making you feel low or anxious.
- Physical exercise – there is a lot of research that shows the importance of exercise for good mental health and for relieving feelings of stress and anxiety. If your mobility has been affected by your brain injury, ask your GP or physiotherapist about what types of exercise they would recommend.
- Relaxation and breathing techniques – if you are feeling stressed and anxious your breathing may become quick and shallow. This can feed feelings of anxiety. Learning slow and deep breathing techniques can help induce feelings of calm.
- Other relaxation techniques include visualisation (for example: imagining yourself in a safe and tranquil place) and progressive muscular relaxation. An internet search or a local class will give you more details on these techniques.
- Mindfulness is a meditative technique which many people find is effective for managing feelings of stress and low mood. There are lots of mindfulness resources online and local classes available in many communities.
- Eating a balanced, healthy diet, limiting your intake of alcohol and caffeine and getting good quality sleep are important for overall wellbeing.
- Try to set goals for yourself that are realistic and manageable. If you are finding it difficult to set goals at the right level for yourself, ask any professionals supporting your recovery for guidance.
- Also, staying focused on making step-by-step progress after your brain injury may help to keep you in a positive frame of mind.

Adjusting to life after brain injury means arriving at a point of accepting who you are now and how life has changed. It is a journey that takes time. It is important to be kind to yourself, to allow yourself enough time and to seek support from other people.
Treatments for depression and anxiety
- The first step is usually to make an appointment to see your GP. They will advise you on the best treatment for depression or difficulties with anxiety.
- They may suggest a referral to a registered Psychologist or an accredited Psychotherapist or Counsellor for ‘talk therapy’ (psychotherapy).
- The GP may also suggest medication.
- For some people, the GP may recommend a referral to a Psychiatrist, a medical specialist in the diagnosis and treatment of mental health difficulties.
Summary of key points
- Many people feel low, depressed or anxious after a brain injury.
- There are a range of options for effective treatments and for ways to help yourself.
- Things such as setting and working towards realistic goals, getting into a routine, talking about your feelings to someone you trust and finding ways of managing how you feel, may be of benefit.

Help and information
If you have any concerns about depression or anxiety, it is important to talk to your GP. It may help to ask a family member, friend or support worker to go with you.
Headway offers community-based brain injury psychotherapy, counselling and rehabilitation in Cork, Dublin, Kerry and Limerick. t: 1800 400 478
HSE Psychologists or Counsellors – your GP or Public Health Nurse can refer you. HSE t: 1800 700 700 w: www.hse.ie.
Registered private Psychologists – contact the Psychological Society of Ireland. t: 01 472 0105 w: www.psychologicalsociety.ie.
Family Resource Centres provide low-cost or free counselling. t: 01 4200 580 w: www.familyresource.ie.
Accredited private Counsellors are listed online in: www.counsellingdirectory.ie and www.iahip.ie.
If you have strong thoughts of ending your life or harming yourself: tell someone you trust, phone your GP or text ‘help’ to 51444, phone the Samaritans on t: 116 123 or phone Pieta House on 1800 247 247, call 999 or go to Accident and Emergency.